 Continuous positive airway pressure (CPAP) has been the gold standard for the treatment of obstructive sleep apnea since the early 1980s. Despite CPAP’s high degree of effectiveness, some patients just cannot tolerate CPAP. As a result, other types of therapy have been developed to address the needs of these patients.
Continuous positive airway pressure (CPAP) has been the gold standard for the treatment of obstructive sleep apnea since the early 1980s. Despite CPAP’s high degree of effectiveness, some patients just cannot tolerate CPAP. As a result, other types of therapy have been developed to address the needs of these patients.
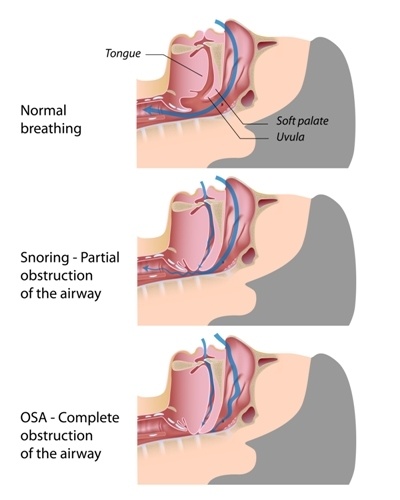
Obstructive Sleep Apnea (OSA)
OSA is a dangerous, chronic breathing disorder which occurs during sleep. Due to a number of factors, the airway collapses and oxygen is prohibited from entering the lungs. This lack of oxygen causes hypoxia, which creates complications for the mind and body.
The effects and complications of OSA include the conditions listed below. Click on each condition to read more about how it is associated with obstructive sleep apnea.
Gasping for or stopping breathing during sleep
Cardiac arrhythmias / congestive heart failure
Poor school or work performance
Brain damage / memory problems
With OSA’s dangerous effects, it is essential that a successful and comfortable form of OSA treatment be initiated for patients who cannot tolerate CPAP.
Lifestyle Changes
Some behavior changes may help reduce the severity of obstructive sleep apnea.
Reduce Alcohol and Nicotine Use
 Alcohol and nicotine make snoring and sleep apnea worse because they significantly relax the airway muscles.
Alcohol and nicotine make snoring and sleep apnea worse because they significantly relax the airway muscles.
It is recommended that you do not consume any alcoholic substances or nicotine products before bedtime.
Lose Weight
Because obesity is a significant factor in the worsening of OSA (about 70 percent of people with OSA are overweight or obese), losing weight will help reduce the severity of OSA. Reducing weight may not cure sleep apnea, but it may enable more treatment options listed below to be more effective.
Positional Therapy
Patients who experience snoring and/or obstructive sleep apnea only when sleeping on their backs may benefit from positional therapy. The premise is to make it uncomfortable for the patient when he rolls onto his back.
Positional therapy products on the market include a device that fits around the neck with the device at the back of the neck. The device can detect sleeping positions, so every time the person is supine, a vibration will occur and will get stronger over time until the person rolls off his back.
Another product is a harness-type apparatus which is worn under night clothes. Inflated bags of air in the back portion of the harness cause discomfort for the patient when he rolls onto his back. If you can sew, a similar apparatus can be composed of a tee-shirt with tennis balls sewn into the back of the shirt.
A 2015 study of positional therapy’s effectiveness found that positional therapy is an easy method for treating supine-dependent sleep apnea on a short-term basis. However, long-term compliance is low.
Oral Appliances
 In 2005, the American Academy of Sleep Medicine recommended that mandibular advancement devices (oral appliances) are acceptable treatment for patients with mild and moderate sleep apnea.
In 2005, the American Academy of Sleep Medicine recommended that mandibular advancement devices (oral appliances) are acceptable treatment for patients with mild and moderate sleep apnea.
Oral appliances are also acceptable for patients with severe apnea who cannot tolerate or who have failed CPAP.
Oral appliances look similar to sports guard and are worn in the mouth during sleep. They pull the lower jaw forward a few millimeters to keep the airway open and prevent the tongue and the tissues in the airway from obstructing the throat.
Oral appliances are well tolerated by patients with mild and moderate OSA. These devices are effective in about 50% of people who have severe apnea. For patients who have extremely severe apnea, a combination of oral appliance and another OSA therapy may treat the apnea more effectively.
Oral appliances are comfortable, portable, easy to travel with, and easy to care for. Compliance rates for oral appliances range from 70-85 percent.
You may have seen boil-and-bite oral appliances in the drug store, whose marketing promises snoring cessation. These in-store devices are not approved by the FDA and you may be doing yourself an injustice by using them. Eliminating snoring by using these store products does not guarantee that you are actually treating your sleep apnea. It is recommended that you seek professional help in dealing with your sleep apnea.
An FDA-approved device is custom-fitted by a qualified dentist. You can find qualified sleep medicine dentists through the American Academy of Dental Sleep Medicine at: http://www.aadsm.org/FindADentist.aspx?1
 The sleep medicine dentist with complete an evaluation, have you fill out a sleep history, will gather other information and then discuss if you are a good candidate for an oral appliance.
The sleep medicine dentist with complete an evaluation, have you fill out a sleep history, will gather other information and then discuss if you are a good candidate for an oral appliance.
If you are a good candidate, he or she will discuss the OA types that would be most effective for your recovery. The dentist will take a mold of your mouth and make a custom-fit device for you.
It can take months before a patient has completed the process but with the high rate of compliance and satisfaction, it is well worth it for this effective treatment modality.
There are over 100 different oral appliances approved by the FDA. For an explanation of the different types of appliances, here is a link comparing 21 different oral appliances. Check them out at http://a360-wp-uploads.s3.amazonaws.com/wp-content/uploads/sleeprev/2015/09/OralAppliancesGuide082015.pdf?a3137e
Oral Pressure Therapy (OPT) by Apnicure
A new technology on the market for treating sleep apnea is oral pressure therapy. This device includes a soft, flexible mouthpiece which sits over the teeth like a mouth guard. Connected to the mouthpiece is slim tubing which is connected to a device which sits on a nearby table.
The machine creates a light oral vacuum, causing negative pressure inside the mouth. This negative pressure stabilizes the tongue and gently pulls the soft palate forward, preventing a collapse of those tissues in the airway.
 OPT is appropriate for anyone with mild, moderate or severe apnea.
OPT is appropriate for anyone with mild, moderate or severe apnea.
The person must be able to breathe through their nose and keep their mouth closed during sleep. It works best for people who have a BMI < 40 kg/m2.
OPT does cause the mouth to release saliva, which is collected in a canister. Rinsing out the canister may be disgusting to some people, but the majority of people who use OPT report that the device is convenient, easy to use and easy to clean.
Expiratory Positive Airway Pressure (EPAP)
Another therapy which has been on the market for a few years is Provent’s EPAP sleep apnea therapy. These are disposable, adhesive-like valves which are taped to the ends of the nostrils before bedtime.
The technology allows a full breath to be inhaled into the lungs, but upon exhalation, the valve on the inside of the nose allows only a limited amount of air to be breathed out. This leaves air inside the nostril and airway, causing a positive pressure inside. This positive pressure prohibits the airway from collapsing.
A 2011 research study led by Dr. Richard Berry and Dr. Meir Kryger to determine the EPAP device’s efficiency revealed that Provent EPAP users had significantly lower apnea-hypopnea index and less daytime sleepiness, compared to a group who did not use the EPAP device. Adherence was excellent and no negative outcomes were reported.
Surgeries
Upper Airway Stimulation (UAS)
Upper airway stimulation is a fairly new surgical procedure for treating OSA, approved by the FDA in April 2014. The UAS is a small device implanted in the upper right chest, under the clavicle. The UAS monitors the breathing patterns of an OSA patient and delivers mild stimulation to the hypoglossal nerve in the airway when the airway collapses. The airway muscles then contract and the throat opens.
Even though surgery does carry a risk and could result in infection or complication, the UAS is less invasive than other surgeries, and there have been no major concerns or difficulties with this therapy.
Pillar Procedure
For those patients with a significant amount of soft palate activity involved in their snoring or OSA, the pillar procedure may be good OSA therapy. During the local anesthetic procedure, small woven inserts are placed into the soft palate to stabilize the palate by making it stiffer.
Multiple studies have shown that the pillar procedure gives a reliable, meaningful improvement in a person’s apnea-hypopnea index, and patients report less daytime sleepiness.
UPPP Surgery
 Whereas the above pillar procedure does not destroy any tissue, the uvulopalatopharyngoplasty (UPPP) does remove tissue from the posterior soft palate and uvula. The tonsils may also be removed during the UPPP surgery.
Whereas the above pillar procedure does not destroy any tissue, the uvulopalatopharyngoplasty (UPPP) does remove tissue from the posterior soft palate and uvula. The tonsils may also be removed during the UPPP surgery.
As in all treatment, surgery is an invasive and risky treatment. Removal of tissue that causes airway collapse will improve the severity of OSA, but one of the difficulties with surgeries is that they only deal with one portion of the airway. There may be other tissue in the nose, mouth or airway which causes blockages.
Surgery intervention needs to be tailored to the individual. This requires the surgery to be exacting in identifying all the tissues causing the OSA. Because this identification does not always occur, and because there may be other factors which influence the snoring and apneas, UPPP surgery is successful in about 40 percent of the cases.
Other Surgeries
Nasal surgery reduces or removes blockages in the nasal cavity;
Hyoid advancement surgery pulls the tongue forward by repositioning the hyoid bone. This prevents the tongue from collapsing into the airway while sleeping;
Tongue reduction surgery removes some of the tongue muscle in the back of the mouth which intrudes into the airway;
Maxillomandibular advancement surgery is a challenging surgery not done very often because of its complications. It requires the precise cutting of the bone and the moving forward of both the upper and lower jaws to create more space in the airway.
Summary
Obstructive sleep apnea is a condition which has too many adverse physical and mental ramifications to ignore. For those who cannot tolerate CPAP therapy, other options are available, from losing weight to complicated surgery. We encourage you to discuss other therapy options with your sleep specialist so you can receive effective and comfortable treatment, helping you regain your health and life.
Sources:
http://sleepdisorders.sleepfoundation.org
RB Berry, MH Kryger, “A novel nasal expiratory positive airway pressure (EPAP) device for the treatment of obstructive sleep apnea: a randomized controlled trial,” Sleep 2011; 3494): 479-485.
GE de Vries, A Hoekema, et al. Usage of positional therapy in adults with obstructive sleep apnea. Journal of Clinical Sleep Medicine, 2015;11(2):131–137.
Image Credit:
www.shutterstock.com


 Excessive daytime sleepiness
Excessive daytime sleepiness



Leave a comment