SAD or OSA?
Since depression is associated with both Seasonal Affective Disorder (SAD) and Obstructive Sleep Apnea (OSA), how can you tell if you have SAD or OSA? Let's look at the various factors which make up both conditions to help you determine which you may be suffering from.
SAD Diagnosis
Having a dip in mood when Daylight Savings Time ends in November is fairly common. When the days get shorter, and we go to work in the dark and come home in the dark, it can darken our mood. This reaction to lack of light is pretty normal, and most people will adjust to winter light and the time change in a short while. There are those, however, who are susceptible to the light changes and suffer from a disorder called Seasonal Affective Disorder (SAD).
According to the Mayo Clinic, SAD is a subtype of major depression and is related to changes in seasons. According to the National Institutes of Health, a patient must have shown depressive symptoms for at least two years before being diagnosed with SAD. Most physicians will complete a physical exam, lab tests, a psychological evaluation, and use the DSM-5 to diagnose SAD and other mental conditions.
Symptoms of SAD
Irritability
Tiredness or low energy
Problems getting along with other people
Hypersensitivity to rejection
Oversleeping
Craving for high carbohydrate foods
Weight gain
Want to “hibernate”
In general, SAD symptoms are not as severe as other types of depression where the person feels hopeless, can’t get out of bed in the morning, or cannot function in daily life. SAD can, however, progress to more serious levels if untreated and/or if the person suffers from more than one type of depression.
Obstructive Sleep Apnea Diagnosis
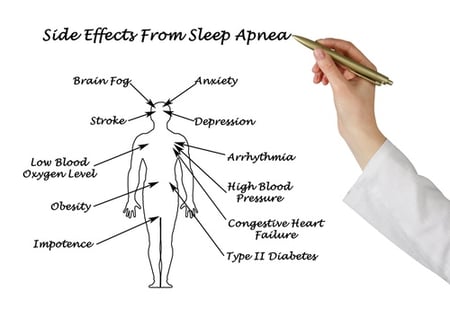 OSA is a chronic, sleep-related breathing disorder which has many adverse, dangerous effects, one of which is depression.
OSA is a chronic, sleep-related breathing disorder which has many adverse, dangerous effects, one of which is depression.
If you snore, gasp for breath during sleep, stop breathing, are obese, have memory problems, are tired or sleepy during the day, or have high blood pressure or another major medical problem, such as heart attack, stroke or diabetes, you may have obstructive sleep apnea.
Your primary care provider may give you a sleep questionnaire such as the Epworth Sleepiness Scale to determine how sleepy you are. Another questionnaire called the STOP-BANG Questionnaire is used to determine what your risk factors are for OSA.
If you are at a high risk for OSA, your physician will refer you to a sleep specialist who will do a physical examination, complete an extensive sleep history, gather other pertinent information, and refer you for either a home sleep study or an in-lab sleep study, called a polysomnogram. In either type of study, equipment will be placed on you that will gather information while you sleep. This information will be evaluated to determine if you have OSA or some other sleep disorder.
Clues
Certain clues like the timing, risk factors, cause, and treatment remedies will help you pinpoint if you are suffering from OSA or SAD, though there are those who may be suffering from both.
Timing of SAD and OSA
SAD begins and ends at about the same time every year. Symptoms start in the fall and continue into the winter months, sapping your energy and making you moody. SAD can cause depression in the sunnier days of spring or summer, but it is less common. In either case, symptoms may start out mild and become more severe as the season progresses.
Depression associated with OSA is year round and is not affected by light or other circadian influences.
Risk Factors of SAD and OSA
There are some major differences in the risk factors for SAD and OSA.
SAD sufferers are more often women than men, and young people have a higher risk of SAD than older adults. Symptoms of depression may worsen seasonally for SAD sufferers. Certain living locations also affect SAD sufferers—those who live far north or south from the equator are more likely to have SAD due to the sunlight shining with less intensity and at an angle.
On the other hand, there are more men OSA sufferers than women, and older adults are more likely to be at higher risk for OSA than younger people. Symptoms of depression do not worsen with the seasons, and locations do not influence OSA depression.
Cause of SAD and OSA
 SAD is caused from three major situations. The reduced amount of sunlight in the winter disrupts human beings’ internal circadian rhythms, which leads to depression in SAD patients. Reduced sunlight can affect both the serotonin levels, which is the brain chemical that affects mood, and the levels of melatonin in our brain chemistry, which also affect our mood, as well as change our sleep.
SAD is caused from three major situations. The reduced amount of sunlight in the winter disrupts human beings’ internal circadian rhythms, which leads to depression in SAD patients. Reduced sunlight can affect both the serotonin levels, which is the brain chemical that affects mood, and the levels of melatonin in our brain chemistry, which also affect our mood, as well as change our sleep.
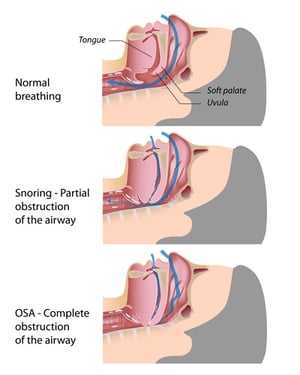
OSA is a sleep-related breathing disorder which occurs when the airway collapses while sleeping. Depression can be an adverse effect caused by a combination of fragmented sleep, oxygen desaturations, and hypercapnia that occurs as a result of the airway being occluded during OSA.
SAD Treatment Remedies
SAD sufferers have several treatment options available to them. Because SAD is caused by a lack of natural sunlight, light therapy is one of the first lines of treatment. This light will give the patient the light they need to reset their circadian rhythms and to function normally.
Some people need light therapy in the morning and some may need light therapy in the evening, so the timing of your light therapy should be determined by your physician. Light therapy can be administered in two ways. You can sit in front of a light box or lamp for 30 minutes to two hours, or you can have a dim light come on in the morning while you are still sleeping. The light will get brighter over time, simulating the sunrise. The method and type of delivery should also be discussed with your physician.
Antidepressants can also be used (with or without light therapy) to treat SAD.
Counseling is also a treatment remedy for SAD (alone or in combination with light therapy and/or antidepressants).
Insomnia and Depression
Research has found that people who have insomnia have a ten-fold risk of developing depression. Those who have the types of insomnia that keep them from falling asleep at bedtime AND from falling back to sleep in the middle of the night have the greatest risk for depression. Women have insomnia more often than men.
It turns out that in many instances, women who actually have OSA are misdiagnosed as having insomnia, and on further evaluation are found to really be suffering from obstructive sleep apnea. If you are someone who has difficulty falling asleep, it would be prudent to discuss this condition with your physician. If you have been prescribed insomnia treatment that is not working—you may actually have OSA.
OSA Treatment Remedies
OSA treatment includes continuous positive airway pressure (CPAP) or similar machine such as an APAP or a BiPAP. These machines blow air into a mask which the patient wears over their nose and/or mouth. The pressurized room-air blown into the mask and airway keeps the airway open during sleep, preventing apneas for occurring.
Other OSA treatment options include (1) oral appliances which move the bottom jaw forward a few millimeters to keep the airway open, (2) surgeries to remove tonsils, adenoids, and other tissues in the mouth and throat which may be causing the airway obstruction, and/or (3) lifestyle changes such as weight loss or positional therapy for those who have apneas only in certain sleeping positions.
Though there are several therapies available for relieving OSA, CPAP is the gold standard for OSA treatment. Your physician will discuss the different therapy methods and determine which is best for your particular situation.
CPAP and Depression
In a 2011 research study led by Dr. Maurice Ohayon of Stanford University, it was found that people with depression were five times more likely to suffer from OSA and other sleep-related breathing disorders. Studies have determined that patients who were treated with CPAP had significant and lasting improvements of their depression symptoms.
 In 2015, research conducted by Dr. David Hillman concluded that CPAP therapy significantly reduced the depressive symptoms of 73 percent of sleep apnea patients.
In 2015, research conducted by Dr. David Hillman concluded that CPAP therapy significantly reduced the depressive symptoms of 73 percent of sleep apnea patients.
Those who used CPAP conscientiously for three months reported that their baseline feelings of self-harm and being better off dead were completely gone and none of the patients were having persistent suicidal thoughts after three months of CPAP use.
Dr. Hillman stated that obstructive sleep apnea is a notoriously underdiagnosed condition and many times is misdiagnosed as depression.
Summary
Whether you are suffering from SAD or OSA, depression is a serious, progressive mental disorder and it is wise to seek help. Psychiatrists and primary care providers are urged to investigate the possibility of OSA being the cause of depression. Finding the real cause of the depression will help you and your doctor find the proper remedy so you can live a life filled with joy and fulfillment.
Sources:
www.mayoclinic.org
http://medical-dictionary.thefreedictionary.com
www.webmd.com
www.sleepfoundation.org
www.aasmnet.org
Image Source:
www.shutterstock.com







Leave a comment