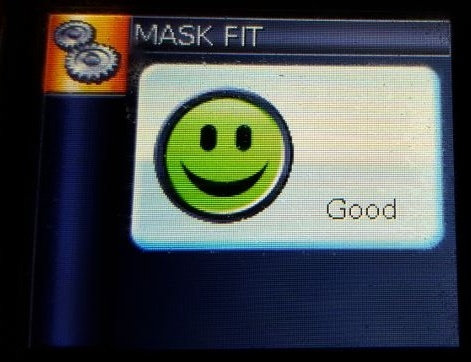
Is your CPAP machine smiling at you in the morning? If so, your CPAP mask is fitting properly and does not have excessive leak. In addition to providing cute faces, the technology of today’s CPAP machines allow patients to follow the progress of their treatment. A smiley face and a frowning face are easy to interpret, but what about all those acronyms attached to numbers? Let’s take a look at some of the more common parameters measured by a CPAP machine.
CPAP
Continuous Positive Airway Pressure (CPAP) is the gold standard treatment for treating obstructive sleep apnea. CPAP devices administer pressurized room air through a hose and mask into a person’s airway to prevent the airway from collapsing during sleep. The amount of pressure prescribed is specific to the person for whom the CPAP device is prescribed.
SDB
Sleep Disordered Breathing (SDB) is an umbrella term to describe respiratory disorders which are characterized by abnormal respiratory patterns or insufficient ventilation during sleep. The SDB category includes apneas, hypopneas, flow limitation, upper airway resistance and snoring.
OSA
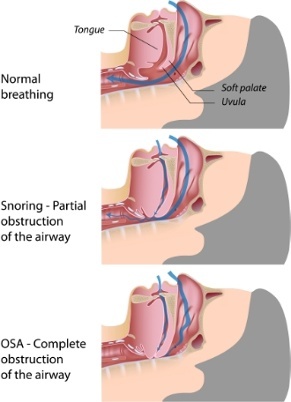
Obstructive sleep apnea (OSA) is one of the most well known and common disorders found in the sleep disordered breathing category.
Apnea
OSA occurs when a person’s airway partially or completely collapses during sleep, preventing air from getting through the airway and into the lungs. The word “apnea” means “without breath” or "no breath." To be classified as an apnea, the respiratory event must reduce the baseline breathing by 90 percent or greater. This basically means that no air or oxygen is getting into the lungs. This causes oxygen desaturations to occur as the body uses its oxygen supply to keep itself alive.
Hypopneas
A hypopnea is also a closing of the airway, but only partially. To be counted as a hypopnea, the airway closure must reduce the baseline breathing between 30 percent and 89 percent.
Apneas and hypopneas must last at least 10 seconds, but the average length of these events is 20-40 seconds. There have been apneas as long as 90 seconds long. When a patient experiences these very long apneas during an all-night sleep study, the sleep technologist monitoring the patient gets very nervous.
AHI
The severity of a patient’s OSA is classified by their AHI (Apnea-Hypopnea Index—A for Apnea, H for Hypopnea), an index that indicates the severity of a person’s OSA. The AHI is the result of calculating the total number of apneas and hypopneas over the sleep time and dividing them by the number of hours of sleep. The higher the AHI, the higher the number of apneas and hypopneas and the more severe the OSA.
AHI Severity Index
Normal 0-5 events/hour
Mild OSA 5-15 events/hour
Moderate OSA 15-30 events/hour
Severe OSA 30+ events/hour
If you see a rise in your AHI, contact your durable medical equipment (DME) company or your sleep specialist to discuss these recent changes.
The below images are readings from CPAP machines. Different machine models will display the information a little differently, but all will use the standard acronyms. 
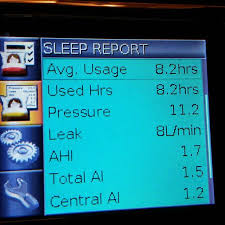
As you can see, the person using the CPAP machine on the left did not have any apneas or hypopneas during the previous night, but the person using the CPAP on the right had 1.7 events per hour. Both of these readings are within normal range.
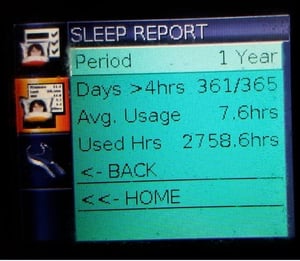
Sleep Reports
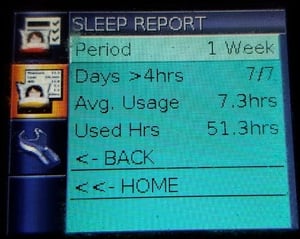
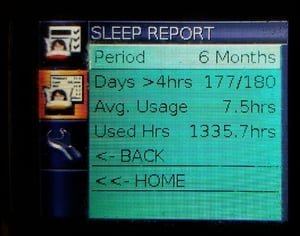
It is important to know the significance of your CPAP readings. Medicare requires patients to use their CPAPs at least 4 hours a night an average of 5 nights a week. Keeping track of your usage will help you stay in compliance with Medicare or other insurance companies that may place usage requirements on the continued availability and insurance reimbursement of the machine.
CPAP machines can display sleep reports covering one day to one year. Below are three readings on the same patient: one week, six months and one year. Notice that the patient was very compliant with using therapy, wearing it 361 days out of 365 and sleeping an average of 7.6 hours per night.
Leak
Every CPAP mask has an exhalation port, a set of holes where air comes out. This air is your used breath, and the holes are there to expel the carbon dioxide you are exhaling. It is dangerous to cover over the exhalation port. This expelled air coming from the exhalation port is called the intentional leak.
There may be a leak coming from a less-than-perfect seal of the mask against your skin. This type of leak is the unintentional leak. Most leaks occur around the eyes, nose or mouth. Mouth breathing will cause a very high unintentional leak.
Total leak is the sum of the intentional and unintentional leak. Leak amount will increase as your air pressure setting increases.

In the example above, leak is at 10 liters per minute, which is well within the 24 L/min maximum leak. Anything over 24 L/min and that green smiley face turns into a red frowning face!
Ramp
Ramp is a comfort feature on some CPAP machines which decreases the initial air pressure when the machine is turned on. This reduced air flow makes it easier to breathe against when you are just getting comfortable and falling asleep. The pressure will gradually increase over a matter of minutes until it is at your prescribed pressure.
By the time the pressure gets full pressure, you will more than likely be asleep. In this example, the ramp time is set at 20 minutes. The CPAP pressure will begin at your chosen ramp start pressure and slowly move up to the prescribed pressure over a 20 minute time period.

Auto
If you have an APAP (Autoset) machine instead of a CPAP, your screen will display something similar to the below image. APAP machines have an upper and lower pressure range (maximum pressure and minimum pressure) instead of a constant pressure as in CPAP. This variable rate allows the pressure to fluctuate during the night to meet the patient’s breathing needs.
The below image shows a maximum pressure of 12.0 and a minimum pressure of 8.0. This means the pressure starts out at 4.0. Over a 40 minute period of time, the pressure slowly rises during the ramp period to 8.0. While the person is sleeping, the pressure will fluctuate between 8 and 12 depending on what stage of sleep the person is in and how much air he/she needs.
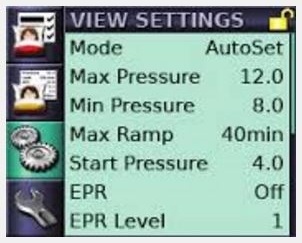
EPR
Expiratory Pressure Relief (EPR) is a feature that decreases the air pressure flow on a variable basis from 1-3 when the patient is exhaling. Breathing against strong air pressure can be disturbing and uncomfortable, and the EPR reduces the air pressure during patient exhalation for more comfort.
Level 1 is the lowest amount of expiratory relief and level 3 is the most available expiratory relief. In the above example, the EPR level is set at 1, but the EPR feature is turned off.
Summary
In the past, patients were not allowed to view their data, but in the past few years sleep medicine professionals have begun seeing the advantage of allowing patients to view their data. Knowing more about their own therapy and seeing the progress encouraged patients to become more interactive with their own treatment and more compliant with therapy.
Sources:
http://healthysleep.med.harvard.edu
http://www.cpaptalk.com/wiki/index.php/Reading_Data
Image Credit:







Leave a comment