.jpg?width=650&name=shutterstock_424762825%20(1).jpg) For treatment of obstructive sleep apnea (OSA), both CPAP and APAP are very effective. The question of which is better depends on a variety of factors.
For treatment of obstructive sleep apnea (OSA), both CPAP and APAP are very effective. The question of which is better depends on a variety of factors.
CPAP (continuous positive airway pressure) emits a continuous stream of pressurized room air into a patient’s mask, which mechanically splints open the airway, to eliminate obstructive apneas during sleep.
The precise CPAP pressure amount is usually determined during an overnight titration sleep study which occurs in a sleep center. As the patient sleeps, the sleep technologist will monitor the patient and increase the air pressure throughout the night until the pressure is reached that eliminates all breathing events and snoring. This will be the ideal pressure, and the patient’s home CPAP device will be programmed with this pressure. The ideal air pressure is the amount of air pressure that is takes to eliminate all apneas, hypopneas, flow limitations and snoring.
If you had a home sleep study done instead of a sleep study done in a sleep center, you may have been prescribed an APAP machine. A home sleep study is not as accurate at detecting apneas as a sleep study in a center monitored by a sleep technologist. As a result of the home sleep study underestimating respiratory events, APAP devices (automatic positive airway pressure—also known as autoPAP or auto-CPAP) are prescribed as the treatment modality because of their flexibility in addressing the patient’s breathing needs more accurately.
APAP is similar to a CPAP in that it also emits pressurized room air into the patient’s airway, but unlike CPAP that only provides one constant pressure, APAP has the added feature of providing a range of air pressure to meet the patient’s particular changing breathing needs throughout the night. APAP is designed with a low pressure setting and a high pressure setting. This range of air pressure in the APAP allows it to fluctuate automatically to the patient’s breathing needs.
How APAP Works
This image shows how APAP works. The image shows normal breathing occurring at the beginning of this graph.
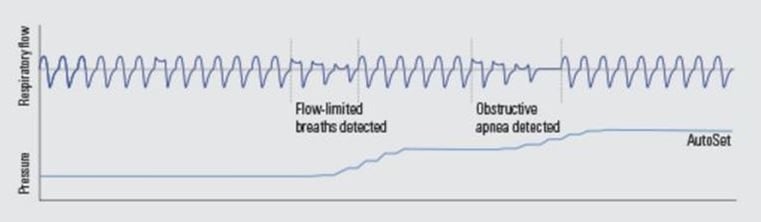
Three reduced, flattened breaths are detected (indicated as flow-limited breaths) and the APAP machine increases automatically to bring the baseline breathing back to normal. The patient then has an obstructive apnea and the APAP again increases just enough to return the patient’s breathing back to normal. With a CPAP device, the pressure is constant and does not adjust itself to the patient’s breathing.
Comparing APAP to CPAP
The below image indicates the thick black line of both a CPAP and APAP. In comparing the CPAP and APAP pressure output, notice CPAP air pressure is constant but APAP pressure rises and falls throughout the night.
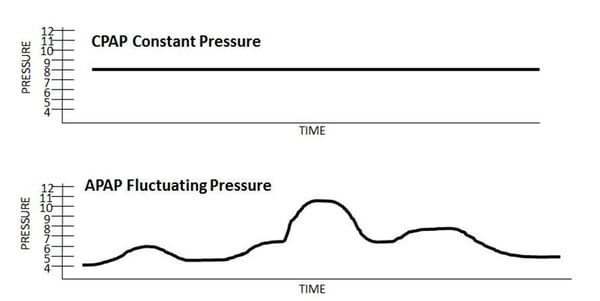 CPAP pressure optimally is set to eliminate obstructive apneas (apneas cause the airway to be entirely obstructed). For many patients, CPAP is the only type of treatment that they need. However, APAP gives the precise amount of air that is needed to eliminate certain types of events. Because of this, the average pressure overall is generally reduced more in APAP treatment than in CPAP treatment, which makes it more comfortable for patients.
CPAP pressure optimally is set to eliminate obstructive apneas (apneas cause the airway to be entirely obstructed). For many patients, CPAP is the only type of treatment that they need. However, APAP gives the precise amount of air that is needed to eliminate certain types of events. Because of this, the average pressure overall is generally reduced more in APAP treatment than in CPAP treatment, which makes it more comfortable for patients.
For example, if the patient is having flow limitation like pictured above where the airway is only partially obstructed, a CPAP machine is going to be giving the patient more air then is necessary to eliminate that flow limitation. This additional pressure via CPAP can be disturbing to patients. The CPAP pressure may also be too high for the patient when the person is initially falling asleep. APAP’s comfortably-reduced pressure increases compliance to therapy.
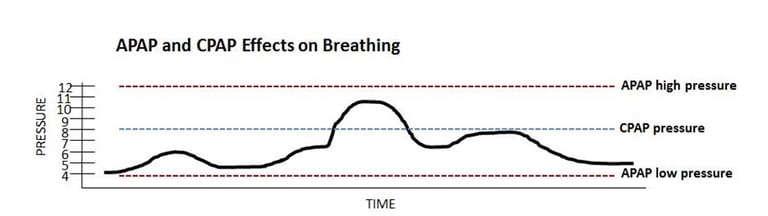
The below image compares APAP’s to CPAP’s effects on respiratory events. For example, let’s say a person had a titration sleep study done which showed that the ideal pressure for eliminating apneas was 8 cm H2O. The CPAP pressure would be set at 8. However, there are many times when a pressure of 8 is not necessary because the airway is not completely obstructed. In this case a lower pressure could be given. And there are times (discussed below) when a person’s respiratory events may exceed a pressure of 8, and thus the person is not getting enough air with CPAP.
Who Benefits from APAP?
Patients may have differing pressure needs during the night for a variety of reasons.
Sleeping Supine
It is generally agreed that when a person sleeps supine (on their back), their tongue and airway muscles will relax and be drawn downward by gravity. This additional pull on the relaxed airway tissues increase the possibility of the airway collapsing. Sleeping supine usually makes sleep apnea worse.
In order to avoid this collapsed airway, the APAP will increase the pressure entering the mask to keep the airway open. When the person rolls back onto their side, the risk of airway collapse is lessened. The APAP machine can then reduce its pressure. With a CPAP treating this type of person, the one constant pressure would be the same for both side position and supine position, thus not creating the ideal treatment for one of the positions.
Allergies, Colds and Respiratory Infections
APAP is also an excellent alternative to CPAP when it comes to allergies, colds, and respiratory infections or congestion. If you have congestion or stuffy nose or other nuisance going on in your nasal cavity, APAP may be better designed to deal with these situations. The APAP will calculate your air intake (through that stuffed nose or plugged up sinuses) and adjust accordingly to deliver the right amount of air pressure to help you breathe.
COPD and Other Compromises
Some people only experience apneas when they are in the sleep stage known as Stage R, where rapid eye movement (REM) sleep occurs. REM sleep is a deep sleep where memory, mind and cognitive functioning are restored. Breathing becomes irregular, blood pressure can spike and temperature defies regulation.
During REM sleep, the muscles of the body are paralyzed, so that we cannot act out our dreams and hurt ourselves or our bed partner. This paralysis (called atonia) decreases the ability of the muscles in the airway to respond and creates more severe apneas and airway blockages.
This atonia affects almost every person’s breathing, making apneas more severe, but for patients with additional respiratory disorders such as COPD or other neuromuscular diseases, atonia during sleep makes it especially hazardous for them. During REM sleep the APAP device will increase its pressure (as shown in the image above) to compensate for these impaired muscles.
Weight Loss/Gain and other Trending Patterns
APAP is an excellent modality for long-term trending patterns. If a person loses or gains a significant amount of weight, a CPAP’s constant pressure setting may eventually be too strong or too weak for the patient’s needs since the CPAP pressure was set when the patient weighed more or less. APAP adjusts automatically to any weight gain or loss that may occur over a long period of time.
Alcoholic Drinking
Consuming alcohol near bedtime increases the severity of obstructive sleep apnea. A CPAP pressure may not be adequate to keep the airway open, but APAP’s flexibility to adjust to the precise level of airway resistance level keeps the airway open.
Costs
Because APAP is the more sophisticated device, the cost of APAP will exceed CPAP’s cost. On average, a CPAP machine costs around $795.00 and an APAP machine costs around $995.00. Since APAP machines can be set as CPAP machines (by setting both the higher pressure setting and low pressure setting at the same number), the APAP machine has an advantage over CPAP devices. In the long run, APAP may be the better and more cost-effective machine for long-term use.
Summary
CPAP and APAP are both excellent therapies for addressing obstructive sleep apnea. Which is better for a particular patient depends on a variety of factors including
cost
sleeping position
variability and types of breathing obstructions
severity of other respiratory conditions (COPD)
the patient’s propensity for allergies or colds
the need for pressure changes over a long period of time.
If you suspect you have obstructive sleep apnea, or have been diagnosed with OSA and are using a machine that is not meeting your breathing needs, contact Sleep Resolutions for resolution of your breathing disorder. We are here to help.
Sources:
www.cpap.com
www.sleepeducation.org
www.sleepapnea.com
Image Credit:
www.shutterstock.com
www.resmed.com







Leave a comment